Bone Loss Dental Implant Solutions are one of the most common reasons patients are told that dental implants are “not possible.” For many people, this comes after years of tooth loss, gum disease, failed dental work, or long-term denture use. However, thanks to major advances in maxillofacial surgery, bone loss does not have to mean the end of implant treatment. At Maxillofacial & Zygoma Implant Center, led by Prof. Dr. Celal Çandırlı, we specialise in innovative, evidence-based solutions that restore fixed teeth and confident smiles — even in complex, high-bone-loss cases.
This comprehensive guide explains why bone loss happens, how it affects implant treatment, and which advanced options may allow you to receive safe, stable, long-term dental implants even after severe jawbone resorption.
What Is Jaw Bone Loss? Bone Loss Dental Implant Solutions
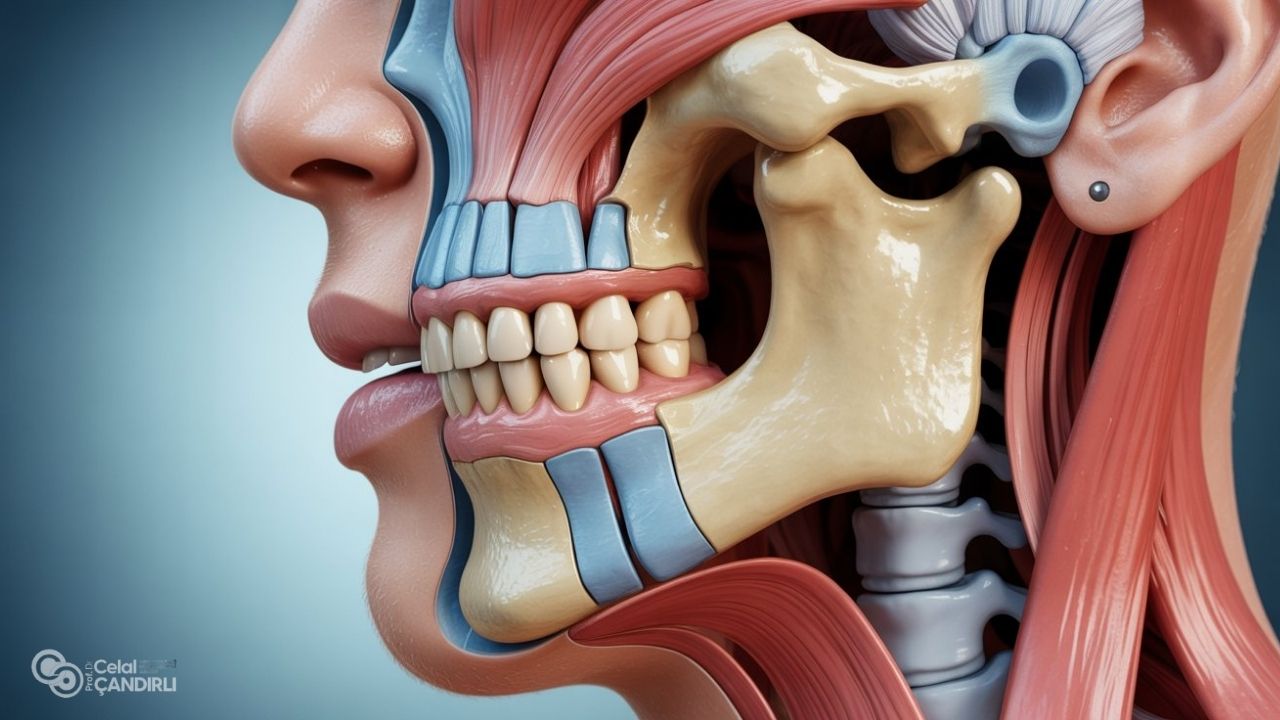
Jawbone is a living tissue that depends on stimulation from natural teeth. When teeth are lost or removed, the bone in that area gradually shrinks — a process called bone resorption. Over time, the upper and lower jaws may lose volume, height, and width, which can create a “sunken” facial appearance, loosen dentures, and make traditional implants difficult or impossible using standard techniques.
Common Causes of Bone Loss in the Jaw
- Long-term missing teeth
- Advanced gum disease (periodontitis)
- Ill-fitting dentures causing chronic pressure
- Trauma or jaw injury
- Failed previous implants or bone grafts
- Congenital or developmental jaw deformities
- Systemic conditions that affect bone density
The longer teeth have been missing, the greater the likelihood and severity of bone loss — especially in the upper jaw, where bone is naturally thinner and softer.

How Bone Loss Affects Dental Implants? Bone Loss Dental Implant Solutions
Traditional implants rely on stable jawbone support. When bone density or volume is insufficient, implants may not integrate properly or may lack long-term stability. In the past, this meant dentures were the only option. Today, highly advanced techniques allow our team to create strong support, even when very little bone remains.
Advanced Bone Loss Dental Implant Solutions
Under the care of Prof. Dr. Celal Çandırlı, each case is evaluated individually using 3D imaging, digital planning and clinical expertise. Depending on your anatomy and treatment goals, your plan may include one or more of the following approaches.
1. Bone Grafting for Dental Implants
Bone grafting increases the amount of bone in areas that have resorbed. Grafting materials may be obtained from your own bone or biocompatible graft substitutes. Over time, the graft integrates with the existing bone, creating a more stable base for implants.
Bone grafting is often recommended when:
- The ridge is too thin or low
- Moderate bone loss is present
- Long-term stability is required for single implants or bridges
Healing time varies but typically ranges from several months before implant placement.
2. Sinus Lift (Sinus Augmentation)
In the upper jaw, bone loss may extend into the maxillary sinus area. A sinus lift raises the sinus membrane and places bone material beneath it, increasing bone height for implant anchorage. This procedure is especially useful for the posterior (back) upper jaw.
3. Ridge Expansion
When the jaw ridge is too narrow, ridge expansion widens the bone to allow safe implant placement. This technique may be combined with grafting or staged with implant placement depending on case complexity.
4. Short or Tilted Dental Implants
In selected cases, shorter or strategically angled implants can make use of available bone while avoiding anatomical structures. Digital planning is essential to ensure optimal stress distribution and longevity.
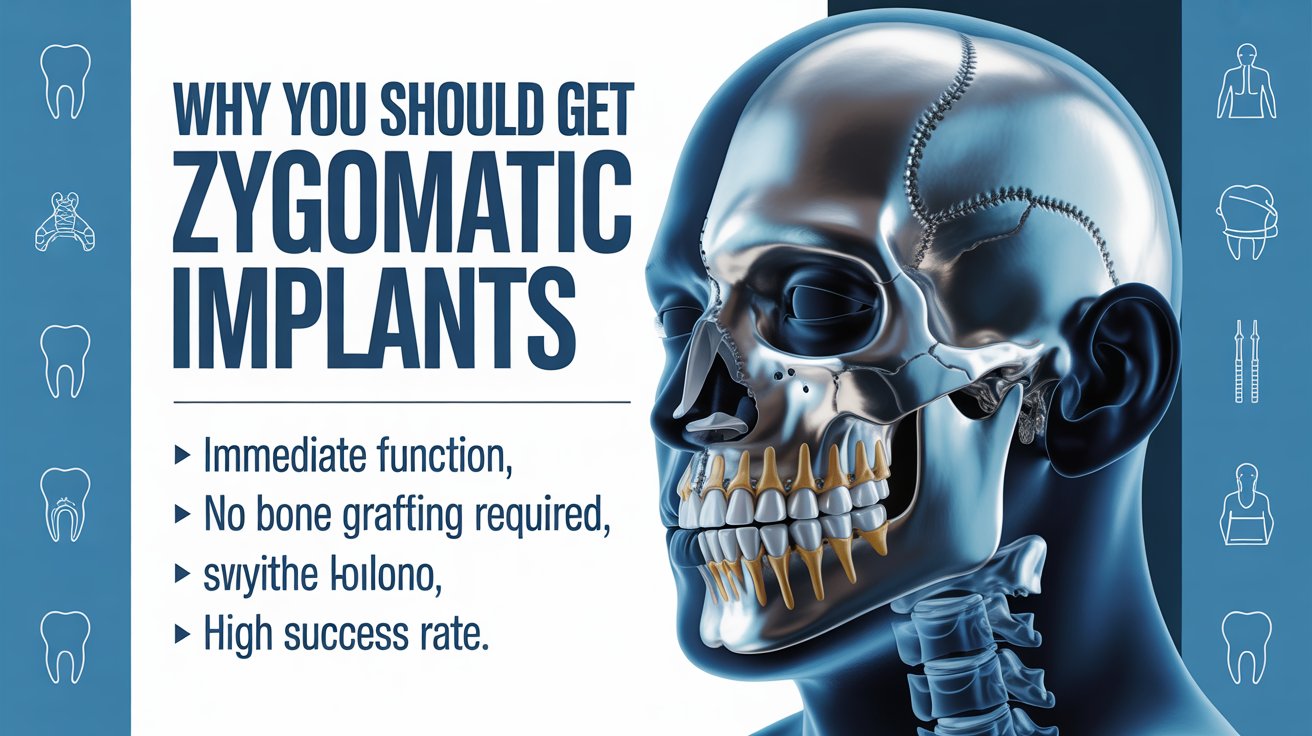
5. Zygoma Implants — A Breakthrough for Severe Bone Loss
For patients with severe upper jaw bone loss, zygomatic implants offer one of the most reliable and predictable solutions. Instead of being anchored in the maxillary bone, these longer implants are anchored securely into the zygomatic (cheek) bone, which remains dense and strong — even when the upper jaw has resorbed significantly.
This makes zygoma implants highly suitable for patients who have:
- Extreme bone loss in the upper jaw
- Failed or rejected sinus lifts or bone grafts
- Long-term denture use
- Multiple missing or failing teeth
- Combined functional and aesthetic concerns
In many cases, zygoma implants eliminate the need for extensive grafting and allow faster restoration with fixed teeth — dramatically improving chewing, speech and appearance.

Zygoma Implants vs. Bone Grafting — A Comparison
| Bone Grafting + Conventional Implants | Zygoma Implants |
|---|---|
| Requires healing time before implants | Often allows earlier tooth placement |
| Best for mild–moderate bone loss | Ideal for severe bone loss |
| Multiple surgeries may be needed | Fewer procedures in many cases |
| Implants placed in jawbone | Implants anchored in cheekbone |
| Long-term success depends on graft integration | Excellent stability in dense zygoma bone |
During consultation, Prof. Dr. Celal Çandırlı will determine which approach best suits your condition, goals and health profile.
Full-Arch Rehabilitation for Bone Loss Dental Implant Solutions
Many bone loss patients also require full-arch reconstruction — replacing all teeth in the upper jaw, lower jaw, or both. Using a combination of conventional, tilted, or zygomatic implants, fixed bridges can be placed to restore natural function and aesthetics.
Benefits include:
- Permanent fixed teeth
- No rocking, slipping, or adhesives
- Improved chewing efficiency
- Greater comfort and confidence
- Support of facial structure
Your Treatment Journey at Maxfax Zygoma Center
Your treatment is tailored to you — never a generic plan. Care is led personally by Prof. Dr. Celal Çandırlı with a structured, patient-centered approach.
Step 1 — Comprehensive Consultation
We assess your dental history, medical background, goals and expectations. High-resolution 3D imaging is performed to evaluate bone quality and anatomical structures.
Step 2 — Digital Planning & Simulation
Advanced planning software allows precise positioning of implants and prosthetics, ensuring accuracy and predictability before treatment begins.
Step 3 — Surgical Phase
Depending on your case, this may include bone grafting, conventional implants, zygoma implants, or a combination. Patient safety and comfort are always prioritised.
Step 4 — Temporary & Final Teeth
In suitable cases, temporary fixed teeth may be placed early. Once healing is complete, custom-designed final restorations are fitted for long-term function.
Step 5 — Ongoing Care & Follow-Up
We support you through recovery and long-term maintenance, helping you protect your investment and oral health.

Who Is a Candidate for Bone Loss Dental Implant Solutions?
You may benefit from advanced dental zygpma implant treatment if you have:
- Severe or long-term bone loss
- Loose or uncomfortable dentures
- Multiple loose or failing teeth
- Difficulty chewing or speaking
- Jaw or facial collapse due to bone loss
- Previous failed implant or graft attempts
Even if you have been told implants are “impossible,” a specialist maxillofacial assessment may reveal options others have overlooked.
Why Choose Prof. Dr. Celal Çandırlı?
Prof. Dr. Celal Çandırlı is a leading maxillofacial surgeon with extensive experience in complex implant rehabilitation and zygoma implant surgery. His approach combines surgical precision with functional and aesthetic excellence, ensuring treatment plans are safe, scientifically grounded and tailored to each patient’s unique anatomy.
Frequently Asked Questions About Bone Loss Dental Implant Solutions
Bone loss can affect your smile, self-confidence, nutrition and facial structure — but it doesn’t have to define your future. With today’s advanced techniques, including zygomatic and specialised implant systems, many patients can finally achieve fixed, natural-looking teeth again.
To learn more about bone loss dental implant solutions and discover which options are right for you, contact the Maxillofacial & Zygoma Implant Center and schedule a consultation with Prof. Dr. Celal Çandırlı. A confident, stable smile may be closer than you think.
How do you treat bone loss in dental implants?
Treatment for bone loss around dental implants depends on the cause and severity. In early stages, improving oral hygiene, treating gum inflammation, and performing professional cleanings may stabilise the area. In more advanced cases, bone regeneration procedures, soft-tissue management, or replacing the prosthetic design to reduce pressure on the implant may be required. When bone loss is severe or infection is present, the implant may need to be removed and the site reconstructed before placing a new implant. A specialist maxillofacial evaluation is essential to determine the safest and most predictable treatment plan.
How to restore bone loss in teeth?
Bone loss around natural teeth is usually caused by gum disease (periodontitis). Treatment begins with deep cleaning to remove bacteria, followed by ongoing periodontal maintenance. In selected cases, guided bone regeneration or bone grafting can help rebuild lost bone support. Treating gum disease early is the best way to stop or slow bone loss progression and protect both teeth and jawbone.
Can you have a dental implant if you have bone loss?
Yes — many patients with bone loss can still receive dental implants. Mild to moderate loss may be corrected with bone grafting or sinus lift procedures. For severe upper-jaw bone loss, advanced options such as zygoma implants or tilted implants may eliminate the need for large grafts. Suitability is determined using 3D imaging and specialist assessment so that implant stability and long-term success can be ensured.
Can a failing implant be saved?
Some failing implants can be stabilised if the problem is detected early, especially when inflammation is limited to the gums. However, if significant bone loss, mobility, or deep infection develops, the safest option is often to remove the implant, treat the site, and rebuild the bone before replacing it with a new implant. Attempting to keep a severely failing implant can lead to further bone loss and complications.
What happens if you don’t have enough bone for dental implants?
If there is not enough bone for standard implants, several solutions are available. These include bone grafting, sinus lift augmentation, ridge expansion, short or tilted implants, and in severe upper-jaw cases, zygoma implants anchored in the cheekbone. Modern maxillofacial techniques mean most patients can still achieve fixed-tooth rehabilitation even with advanced bone resorption.
What is the 3/2 rule for dental implants?
The “3/2 rule” is a guideline used in implant planning and refers to ideal spacing and prosthetic design to help distribute biting forces safely. It is one of several biomechanical principles used to protect the implant and surrounding bone. Final planning should always be done by an experienced implant surgeon using clinical assessment and digital imaging, rather than relying on general rules alone.
What are the alternatives to bone grafts for dental implants?
Alternatives include short implants, tilted implants, immediate-load full-arch systems, and zygoma implants that anchor into the cheekbone rather than the resorbed upper jaw. These techniques may avoid or greatly reduce the need for bone-grafting procedures while still providing strong, fixed teeth for suitable patients.
What is the fastest way to increase bone density?
There is no instant way to increase jawbone density. In dentistry, bone regeneration occurs gradually through guided bone grafting, sinus augmentation, or stimulation from stable implants. For general skeletal health, balanced nutrition, calcium and vitamin D intake, weight-bearing exercise, and medical management of bone-loss conditions may help — but jawbone rebuilding for implants requires professional surgical treatment and time for healing.
How much bone loss is too much for implants?
There is rarely a point where bone loss makes rehabilitation impossible — but it does change the type of treatment required. Severe upper-jaw bone loss may make standard implants unsuitable, yet zygoma implants or combined advanced techniques can still provide stable, fixed solutions. The key is accurate diagnosis with 3D scans and planning by a specialist who routinely treats complex bone-loss cases.